Acute Pancreatitis: Causes, Symptoms, Treatment
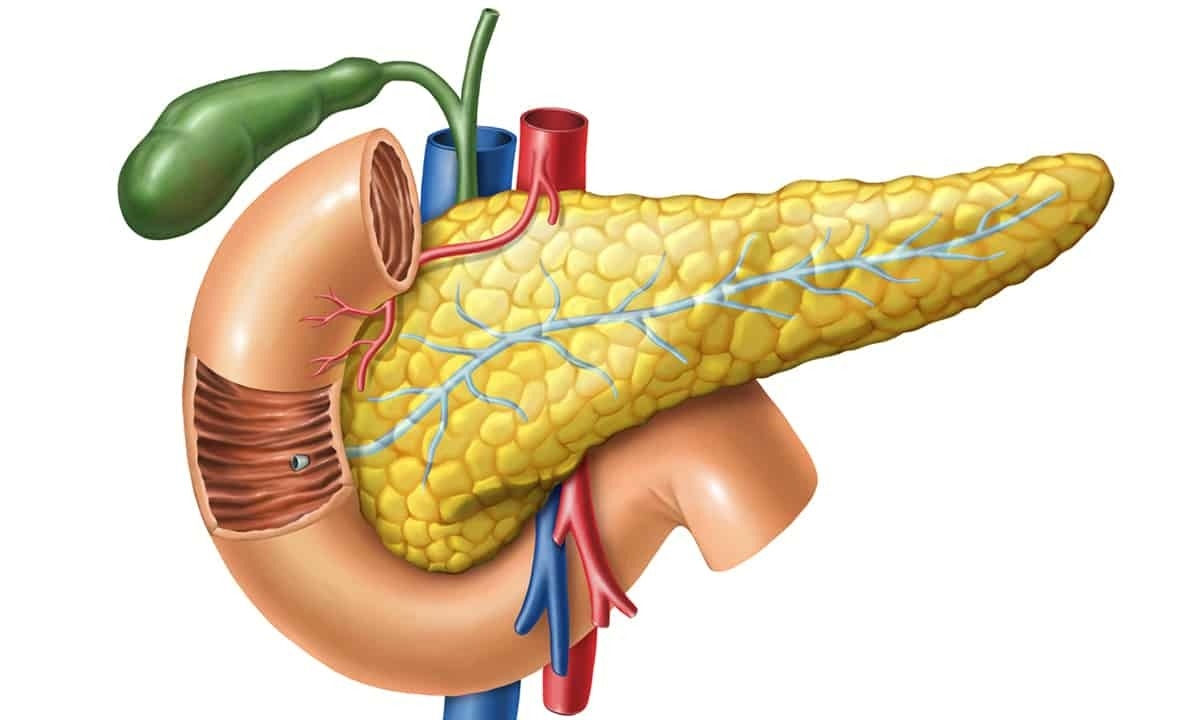
While it is possible to live without a pancreas, it is nevertheless a versatile organ that plays a role in both the endocrine system and the digestive system. Nestled behind the stomach in the upper abdomen, this long and flat gland generates enzymes that help the body regulate blood sugar levels, aid in digestion, and neutralize stomach acid after food leaves the stomach for the duodenum and the small intestine.
There are numerous conditions that can threaten the pancreas, and surprisingly most of them can potentially be avoided through living an active and healthy lifestyle. Diabetes, while not precisely a disease of the pancreas, is one malady that can occur that involves the immune system attacking the pancreatic cells that produce insulin. Another pancreas-related disease that affects tens of thousands of Americans every year is acute pancreatitis.
What is Acute Pancreatitis?
In general terms, pancreatitis is the name for the condition where the pancreas has become inflamed. As with any organ or tissue in the body, inflammation is actually triggered as an immune response to the presence of pathogens or other harmful irritants. The ultimate goal of inflammation is to eliminate any foreign elements that have the potential to cause cell injury. Once the irritant has been eliminated, the body then initiates repairs to any damaged tissues.
There are two main types of pancreatitis: acute and chronic. Acute pancreatitis comes on suddenly and is often a singular event related to a particular trauma or stimulus. Acute pancreatitis may happen once and not return, or it can be a recurrent problem that happens as a response to the same stimuli. Over time, acute pancreatitis can turn into the other major type: chronic pancreatitis.
Chronic pancreatitis is the same basic condition as acute pancreatitis, but it persists over the long term and remains an ongoing problem. When unchecked and untreated, acute pancreatitis can develop into a chronic condition. The long-term inflammation will eventually begin causing irreversible damage to the pancreas, and this damage continually makes the organ less functional and opens the rest of the body up to a variety of other health problems.
At the core of both types of pancreatitis is essentially a mistaken function. Enzymes produced by the pancreas are normally secreted into the bloodstream (insulin, for example) or the digestive tract (lipase, amylase or trypsinogen, for example) in order to be activated and serve their functions. When someone has pancreatitis, however, these enzymes are activated prematurely and begin to actually damage the pancreas itself.
What are the Causes of Acute Pancreatitis?
Doctors and scientists currently don’t know exactly why these enzymes are inappropriately activated in some people and then start to damage their pancreas. The underlying cause of acute pancreatitis may still be a mystery, but there are a number of health conditions that have been identified and are generally accepted as causes:
Gallstones
At around 40% of cases, the most common cause of pancreatitis is gallstones. The gallbladder is a small organ that primarily serves as a reservoir for bile secreted by the liver. Sometimes, when the composition of the bile is abnormal, small concretions called gallstones can form in the gallbladder; these same stones can then leave the gallbladder via the common bile duct and potentially block the duct. The blockage can thus force pancreatic enzymes to remain in the pancreas rather than flow naturally into the digestive tract. This backup of enzymes in the pancreas can then lead to premature activation and subsequent inflammation (sometimes referred to as gallstone pancreatitis).
Metabolic Disorders
Metabolism is the means by which the body transforms food into energy, and a metabolic disorder is any condition that disrupts that process as well as the balance of substances that are necessary for keeping a body healthy. Hypertriglyceridemia (having too many triglycerides in the blood) is one example of a metabolic disorder that can lead to pancreatitis. Other examples include hypercalcemia (too much calcium) and malnutrition.
Infection
It is estimated that approximately 10% of cases of acute pancreatitis are caused by some type of infection. As alluded to earlier, when the body detects a pathogen (such as an infectious agent), it triggers inflammation in order to eliminate the pathogen. Viral infections like mumps, Coxsackie B, and hepatitis B are the most common causes, but bacterial infections such as salmonella can also be the culprit.
Pancreatic Cancer
Having pancreatitis can actually increase the chances of developing pancreatic cancer, but it also works the other way; pancreatitis, especially hereditary pancreatitis, can also be a complication of pancreatic cancer.
Cystic Fibrosis
While rare, cystic fibrosis is another condition that can potentially lead to acute pancreatitis. In patients with cystic fibrosis, a genetically inherited faulty protein related to the production of mucus doesn’t function properly; as a result, the normally slick mucus that lines and protects many organs becomes more viscous. This thicker mucus, when present in the digestive tract, can cause a blockage in the pancreatic duct that can lead to inflammation.
Over time, doctors have discovered that 15% to 25% of pancreatitis cases are considered idiopathic; in other words, the cause of up to 25% of cases is either unknown or unattributable to a specific cause. The above health conditions have been shown to have a strong relationship to pancreatitis, but doctors have also uncovered other factors that can also lead to pancreatitis over time. The following risk factors are known to cause someone to be much more susceptible to developing pancreatitis (as well as a wide variety of other health problems):
Alcohol Abuse
Second only to gallstones, heavy alcohol consumption has been identified as a primary cause of pancreatitis. When alcohol is consumed, special cells in the pancreas called acinar cells metabolize the alcohol and toxic byproducts are produced. Though the exact relationship is still being studied, it has been theorized that these byproducts lead to increased production of digestive enzymes that can then cause their premature activation. Once activated inside the pancreas, these enzymes actually begin to digest the pancreas itself, causing damage. In chronic pancreatitis, this damage over time becomes permanent.
Obesity
Obesity continues to be an increasingly widespread problem in the United States, and the effect of obesity on the pancreas is equally widespread. The pathway from obesity to acute pancreatitis can look very different depending on the patient but research thus far is unclear on there being a direct connection. What is generally accepted, however, is that obesity increases the likelihood of developing gallstones and other health conditions associated with pancreatitis.
Smoking
Current research about the effect of smoking on the potential to develop pancreatitis is still nascent, but all indications are that smoking increases the chances. It appears that nicotine has a similar effect on the pancreatic acinar cells as alcohol. For this reason, the combination of smoking and alcohol use is thought to be particularly toxic and dangerous.
What are the Symptoms of Acute Pancreatitis?
Both acute and chronic pancreatitis share some symptoms, but they also differ in some ways. One of the key differentiators of acute pancreatitis is that it comes on suddenly. Those with chronic pancreatitis will likely recognize the symptoms of acute pancreatitis as they would have preceded the onset of the chronic type. The following are some of the most common symptoms of acute pancreatitis:
- Abdomen that is either tender or swollen
- Nausea
- Vomiting
- Fever
- Faster than normal heartbeat (tachycardia)
- Reduced appetite
- Chills
- Trouble breathing
- Upper abdominal pain (epigastric)
- Can last for days
- May spread to the back
- May be either mild or severe
- Can last for days
Though these symptoms are fairly common, they are rarely all or mostly present. As with most conditions, different patients may experience different symptoms at different times. For many patients, upper abdominal pain is the only symptom that presents. Regardless, in the majority of cases, patients with acute pancreatitis look visibly ill.
Complications with Acute Pancreatitis
Because of how central pancreatic function is to our bodies, and because of how those functions are related to many other body systems, there are a variety of complications that may arise for those patients who have been diagnosed with acute pancreatitis. Like acute pancreatitis itself, many of these possible complications can be serious and even life-threatening. Below are some of the most common complications that may emerge from either acute or chronic pancreatitis:
Pancreatic Cancer
Over time, chronic inflammation of the pancreas greatly increases the possibility of developing pancreatic cancer due to the accumulated damage of pancreatic tissues.
Pseudocyst
This unique type of cyst can begin to collect fluid and other debris in some patients with acute pancreatitis; the development of a pseudocyst can lead to a dangerous rupture as well as infection or an obstruction of the pancreatic ducts.
Infection
In addition to being a potential cause of acute pancreatitis, various infections can also be a complication. The presence of inflammation causes the pancreas to be much more vulnerable to viruses and bacteria. Pancreatic infections are generally serious and may even require surgery to remove infected tissue in cases of severe pancreatitis.
Malnutrition
As a result of pancreatic inflammation, the numerous digestive enzymes the body uses to break down foods are reduced. The net effect of fewer digestive enzymes can result in malnutrition since the body can’t absorb all the nutrients it needs to function properly.
Kidney Failure
In some patients with severe acute pancreatitis, the damage resulting from the production of too many enzymes can ultimately cause a series of problems that eventually can lead to kidney failure.
Lung Problems
One of the side effects of acute pancreatitis is a change in lung function known as hypoxemia that inhibits the body’s ability to effectively oxygenate the blood.
Diabetes
As a component of its endocrine function, the pancreas secretes the vital hormone insulin into the bloodstream to regulate blood sugar levels. Patients with pancreatitis (typically chronic) are more likely to develop diabetes because of damage to the cells that actually produce the insulin.
How is Acute Pancreatitis Treated?
Depending on the severity of acute pancreatitis, treatment may vary. Many people who develop mild acute pancreatitis have a form that typically goes away after a few days with proper treatment and adequate rest. In more severe cases, other treatment options may be considered. Here are some common treatments:
- Fluid Replacement: When a person has acute pancreatitis, the body may utilize a lot of fluids in order to repair damage to the pancreas. As a result, many patients experience dehydration and require intravenous fluid replacement therapy.
- Pain Management: The abdominal pain associated with pancreatitis can become quite severe, so managing the pain with over-the-counter analgesics is typical.
- Fasting: Because of its metabolic function, continuing to eat may prolong the inflammation in the pancreas. To combat this, the doctor may require the patient to fast for two or three days in order to give the pancreas time to rest.
- Surgery: If the pancreatitis is determined to be related to gallstones (which is often the case), the doctor may recommend removing the gallbladder (cholecystectomy). For other patients with more severe cases, all or part of the pancreas itself may need to be removed. Endoscopic surgery via ERCP (endoscopic retrograde cholangiopancreatography) may also be an option to remove a blockage or relieve pressure in the area.
- Medication: Some cases of acute pancreatitis are caused by a bacterial infection; in these cases antibiotics may be prescribed.
Tips for Preventing and Managing Acute Pancreatitis
The good news about acute and chronic pancreatitis is that for the majority of people they can be avoided. Doctors have uncovered a variety of lifestyle choices that can substantially reduce the chances of developing pancreatitis:
- Avoid or reduce heavy drinking
- Avoid smoking
- Maintain a healthy weight through regular exercise
- Modify your diet to prevent gallstones:
- Reduce intake of saturated fat (red meat, cheese, butter, etc.)
- Reduce intake of sugary foods
- Increase consumption of fruits and vegetables
- Snack on healthy nuts like peanuts and cashews
If you already have pancreatitis, the same basic concepts still apply in terms of diet and exercise. But for those who have already had a flare up of pancreatitis, the recommendations are more strict: stop drinking and smoking. Continuing to drink and smoke could be potentially life threatening.
Gastroenterologist Appointment
There are approximately 275,000 hospitalizations every year in the United States for acute pancreatitis; that makes it one of the most frequent causes of hospitalization among gastrointestinal disorders. If you have been experiencing symptoms of acute pancreatitis, you should see a doctor as soon as possible. While many cases are non-serious and treatable, it remains an essentially dangerous condition. Contact us at Cary Gastroenterology Associates to make an appointment to speak with a gastroenterologist.