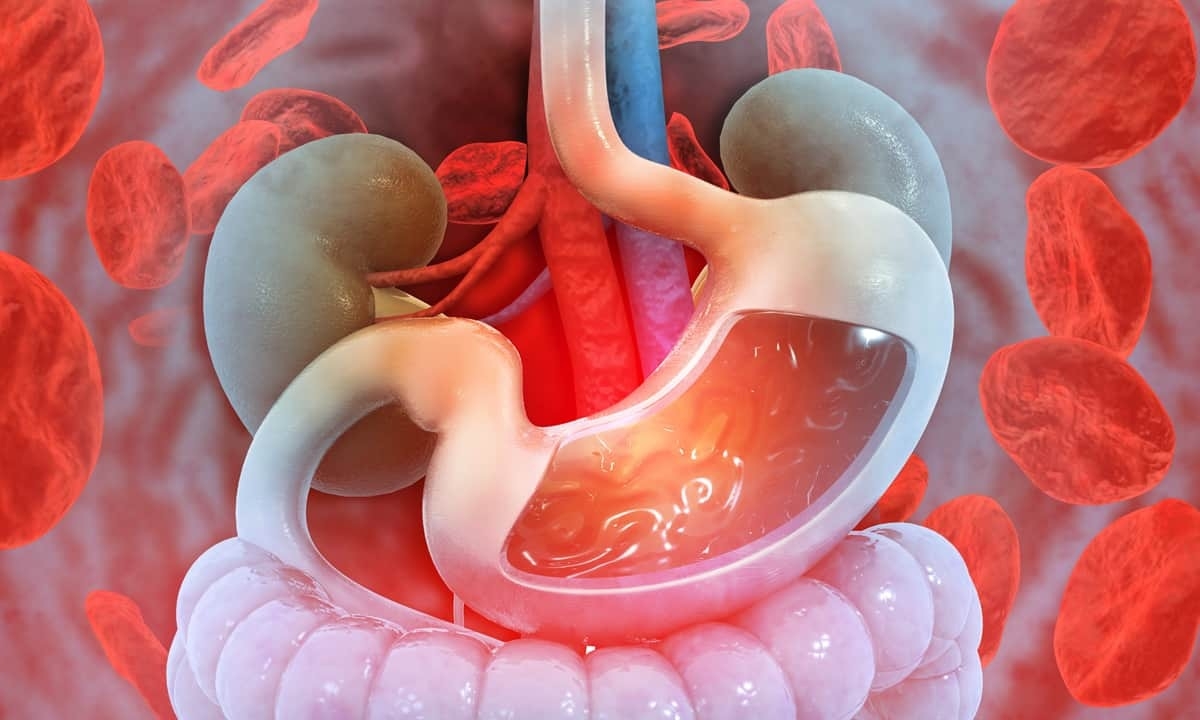
Possible Causes of Gastrointestinal Bleeding
Sooner or later, everyone will have a gastrointestinal problem of some kind. Along with genetics, what we eat, what we drink, and how much physical activity we get are all factors that can have an impact on the digestive process. Mild diarrhea, constipation, and indigestion are familiar symptoms that most people experience regularly and usually can deduce the cause. Gastrointestinal bleeding, on the other hand, is a less common symptom that might not be as straightforward to identify.
Symptoms of Gastrointestinal Bleeding
The gastrointestinal (GI) tract consists of the esophagus, stomach, small intestine, large intestine, rectum, and anus. Bleeding is possible at any point along the digestive tract, and the location of the bleeding can actually influence the way the symptoms manifest. For instance, the color of the blood found in stool can indicate the source of bleeding: upper GI bleeding tends to result in black, tarry stool while lower GI bleeding tends to show up as bright red blood on toilet paper. Below are some other common symptoms and signs:
- blood in vomit
- blood in stool
- vomit that looks like coffee grounds
- abdominal pain or cramps
- dizziness
- faintness
- weakness or fatigue
- shortness of breath
- paleness
Gastrointestinal bleeding can be an isolated incident related to a specific condition, and it is usually a mild concern that resolves without a major medical intervention. In rarer cases, the bleeding can be a greater concern; one example is acute upper gastrointestinal bleeding, a potentially life-threatening condition that may cause shock. In addition to blood being visible in stool or vomit, shock can cause dehydration, a drop in blood pressure, increased pulse, or even unconsciousness. If you experience any of these symptoms, seek medical care immediately.
In people with chronic gastrointestinal bleeding, the blood loss over time can lead to anemia, a condition where the body has fewer red blood cells than normal. Anemia can present as feelings of weakness and fatigue along with shortness of breath. In some cases, blood may be present in the stool without being visibly apparent; this is called occult blood and is only detectable by detailed lab analysis. This kind of chronic GI bleeding typically happens as a result of inflammation or a more substantial digestive problem.
Common Causes of Gastrointestinal Bleeding
Because the digestive tract is such a large and complex body system, there are a wide variety of possible causes of bleeding. Doctors have many methods of diagnosing the problem, including a physical examination, blood test, capsule endoscopy, and scans aided by angiography. Through these various tests and scans, a gastroenterologist can determine the cause and treatment. Below are some common causes of gastrointestinal bleeding based on the location in the GI tract:
Esophagus
- Esophagitis: Esophagitis is an inflammation of the lining of the esophagus that is typically caused by gastroesophageal reflux (GER). GER (like its chronic relative GERD) is the backing up of stomach acid into the esophagus due to a malfunctioning lower esophageal sphincter. The harsh stomach acid can irritate the esophagus enough to eventually cause bleeding for some people.
- Varices: These abnormally enlarged veins located at the base of the esophagus are usually caused by cirrhosis or another type of liver disease. Eventually, the esophageal varices can burst and bleed into the digestive tract.
- Mallory-Weiss tear: Bouts of severe, violent vomiting can cause a Mallory-Weiss tear, a rupture in the mucosal lining of the esophagus near the location it connects to the stomach.
Stomach
- Gastritis: Gastritis is the general term for inflammation of the lining of the stomach. The many reasons for stomach inflammation include Crohn’s disease, inflammatory bowel disease, injury, or the use of nonsteroidal anti-inflammatory drugs (NSAIDs). It can also be caused by lifestyle factors like excessive alcohol consumption and smoking.
- Peptic ulcers: Ulcers in the stomach (also known as gastric ulcers) are most often caused by an infection by a bacteria called Helicobacter pylori. The H. pylori infection leads to inflammation, which in turn can lead to ulcers—painful breaks in the stomach lining that can cause bleeding and a variety of other symptoms.
- Stomach cancer: Stomach cancer can develop in different ways, but they all involve some form of abnormal growth in the stomach lining that can eventually cause bleeding.
Lower Gastrointestinal Tract
- Hemorrhoids: One of the most common causes of lower gastrointestinal bleeding, hemorrhoids are swollen and inflamed veins located near the anus. In addition to being painful and uncomfortable, hemorrhoids can also bleed.
- Anal fissures: Anal fissures are small tears in the lining of the anus that have similar symptoms as hemorrhoids, including the possibility of bleeding.
- Polyps: Colonic polyps are abnormal growths in the colon that are often benign but can sometimes lead to colorectal cancer. When they become irritated and inflamed, they can cause bleeding into the GI tract.
- Ulcerative colitis: This chronic condition involves inflammation of ulcers in either the colon or rectum. In many cases, widespread ulceration causes sufficient bleeding to be detected in the stool.
- Diverticular disease: Diverticula are little pouches that form along the inner lining of the colon; these pouches push out through weak spots in the colon. This is called diverticular disease (or diverticulosis) and can cause a variety of symptoms, including bleeding.
- Angiodysplasia: Angiodysplasia is a condition where blood vessels in the digestive tract become enlarged or otherwise malformed. These fragile vessels are more likely to be irritated and bleed.
Treatment Options
Most cases of gastrointestinal bleeding are relatively easy to diagnose and treat, though of course the type of treatment depends on the underlying cause. In some situations, the method of diagnosis may double as the method of treatment. In a colonoscopy, for example, the doctor may see colon polyps and be able to remove them immediately with special tools mounted on the end of the scope. The doctor can also stop any bleeding by cauterizing the affected area with a heat probe or laser.
When the cause of bleeding is due to an infection or an ulcer, the best option may be medication. This is especially true for problems in the stomach as the stomach acid can exacerbate other conditions. The doctor may prescribe proton pump inhibitors that reduce the production of stomach acid and facilitate healing. In more mild cases, over-the-counter antacids and other medications can reduce inflammation or ease related symptoms.
For most people, GI bleeding is a temporary concern that will go away on its own. As noted above, chronic bleeding can lead to anemia and other complications. If left untreated, more involved treatments may be necessary, like a blood transfusion or intravenous medications or fluids. Gastrointestinal bleeding is also a much bigger concern for anyone who is already on blood-thinning medication.
Contact Cary Gastroenterology
If you have been experiencing gastrointestinal bleeding and you aren’t sure why, it might be time to get checked out by a gastroenterologist. At Cary Gastro, we are dedicated to providing excellent digestive health care. If you would like to speak with a member of our staff, please contact us today to request an appointment.