Recognizing Toxic Megacolon: A Critical Complication of Intestinal Disease
For people with chronic digestive conditions like ulcerative colitis, Crohn’s disease, or persistent gut infections, managing symptoms is often a daily reality. Most patients become familiar with their condition’s patterns and respond accordingly with medication, dietary adjustments, and regular medical care. In rare instances, however, these underlying conditions can develop into a serious complication known as toxic megacolon. Though uncommon, its potential severity explains why doctors may emphasize certain warning signs to patients with inflammatory bowel disease and similar digestive conditions.
What Is Toxic Megacolon?
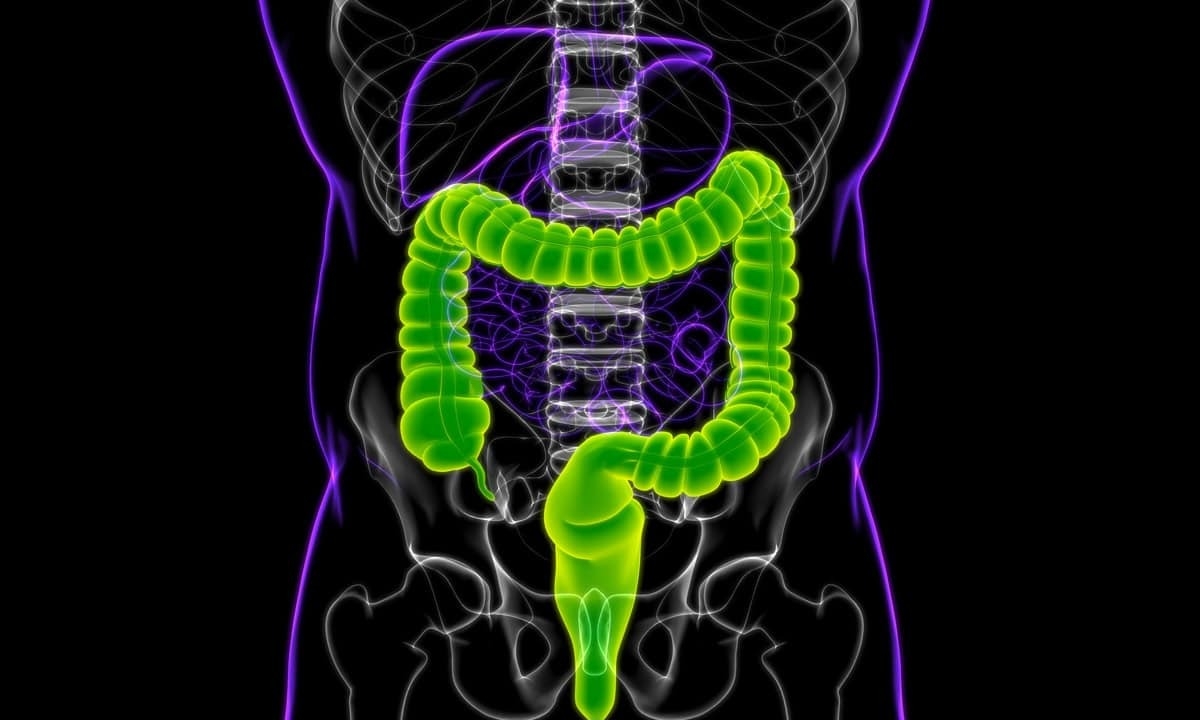
The final section of the digestive tract is the colon (or large intestine), a five-foot-long muscular tube that plays a crucial role in processing waste generated by the body. In addition to being the site where stool forms, the colon absorbs water and electrolytes from digested material before it leaves the body. A properly functioning colon uses rhythmic muscle movements called peristalsis to advance its contents, all while maintaining its standard diameter. This entire process is regulated by a complex network of nerves that communicate between the brain, gut, and surrounding tissues.
Toxic megacolon involves two critical problems occurring simultaneously: extreme enlargement of the colon and systemic inflammation throughout the body. The condition gets its name from the severe dilation of the colon, which can expand to several times its normal width. This dangerous expansion happens when the colon’s muscle layer becomes paralyzed and stops contracting properly. As the colon stretches, its wall becomes dangerously thin and fragile, creating a risk of perforation. If the wall tears, bacteria from the intestine can leak into the abdominal cavity, causing serious infection.
The progression from an underlying condition to toxic megacolon often happens quickly, sometimes within just days. What begins as inflammation or infection in the colon can rapidly worsen when the intestine’s normal protective mechanisms fail. As the condition advances, bacteria may enter the bloodstream from the damaged intestine, potentially causing widespread infection and affecting other organs. When doctors identify toxic megacolon early, treatment can often prevent these complications. However, delayed diagnosis or treatment frequently leads to life-threatening situations that require emergency surgery.1
What Can Cause Toxic Megacolon?
Toxic megacolon typically develops as a complication of existing intestinal conditions rather than arising on its own. Several distinct conditions can create the inflammation and disruption of normal colon function that ultimately leads to toxic megacolon. While some causes are more common than others, all share the potential to severely impact the colon's motility and ability to maintain its structure:
- Inflammatory bowel disease: Both ulcerative colitis and Crohn’s disease can lead to toxic megacolon, particularly during severe flare-ups. Ulcerative colitis poses a higher risk because it directly affects the colon’s lining and muscle function. The chronic inflammation weakens the intestinal wall and can eventually paralyze the muscles needed for normal contraction.
- Clostridioides difficile infection: Commonly known as C. diff, this bacterial infection often occurs after antibiotic use disrupts the normal balance of gut bacteria. Severe cases can produce toxins that damage the colon wall and trigger the extreme dilation characteristic of toxic megacolon.
- Other intestinal infections: Bacterial infections such as Salmonella, Shigella, and E. coli can cause similar inflammatory responses in the colon. These pathogens release toxins that damage the intestinal lining and disrupt normal muscle function, sometimes progressing to toxic megacolon.
- Medication side effects: Certain medications that slow intestinal movement can contribute to the development of toxic megacolon. These include anticholinergics (used for overactive bladder or COPD), opioid pain relievers, and some antidepressants. These drugs can paralyze the colon’s muscles and allow abnormal dilation to occur.
- Ischemic colitis: When blood flow to the colon is reduced or blocked, the resulting oxygen deprivation can damage the intestinal wall and lead to toxic megacolon. This condition is more common in older adults with vascular disease or after certain surgical procedures.
- Ogilvie’s syndrome: Also called acute colonic pseudo-obstruction, this condition causes symptoms similar to an intestinal blockage without any physical obstruction present. It typically affects hospitalized patients recovering from surgery or those with serious medical conditions and can progress to toxic megacolon if not treated promptly.
- Hirschsprung’s disease: This congenital condition involves missing nerve cells in parts of the large intestine, preventing normal muscle contractions. Though it’s usually diagnosed in infancy, milder cases may not be discovered until adulthood and can occasionally lead to toxic megacolon.
- Volvulus: Twisting of the colon can cut off blood supply and create obstruction, leading to rapid dilation and potential development of toxic megacolon if not promptly corrected.2
How to Recognize Toxic Megacolon
Identifying toxic megacolon quickly can make a critical difference in treatment outcomes, as this condition can progress from early warning signs to life-threatening emergency within hours or days. For patients with inflammatory bowel disease, intestinal infections, or other risk factors, distinguishing between a routine flare-up and the development of toxic megacolon requires careful attention to specific symptoms. The key indicators that suggest toxic megacolon rather than a standard exacerbation of the underlying condition include both severe local abdominal symptoms and signs that the entire body is responding to a serious threat:
- Severe abdominal pain and tenderness: Most patients experience significant pain, often described as persistent and diffuse across the abdomen. The abdomen typically becomes extremely tender to touch, and patients may guard or protect the area from pressure.
- Abdominal distention: Visible swelling or bloating of the abdomen occurs as the colon expands beyond its normal size. This distention may develop quickly over hours or days and can be quite pronounced.
- Changes in vital signs: Rapid heart rate (tachycardia) typically exceeds 100 beats per minute as the body responds to inflammation and potential infection. Fever often rises above 101.5°F, though some patients with weakened immune systems may not develop fever despite severe infection.
- Altered bowel habits: While diarrhea is common in the conditions that lead to toxic megacolon, patients may experience a sudden decrease in bowel movements as the colon loses its ability to contract effectively. When bowel movements do occur, they may contain blood or mucus.
- Dehydration and electrolyte imbalances: Fluid loss from diarrhea, decreased oral intake, and leakage of fluids into the abdominal cavity can lead to dehydration. Signs include dry mouth, decreased urination, and extreme thirst.
- Mental status changes: As the condition worsens, confusion, lethargy, or even loss of consciousness may occur due to the systemic effects of toxins entering the bloodstream from the damaged colon.
- Signs of shock: In advanced cases, patients may develop low blood pressure, cool and clammy skin, and rapid, shallow breathing as the body struggles to maintain adequate circulation.
An Overview of Diagnosis and Treatment
Because toxic megacolon can stem from multiple underlying conditions, diagnosis and treatment can vary greatly from patient to patient. Generally, though, diagnosis begins with imaging studies like X-rays or CT scans that can confirm colon dilation. Blood tests can also help evaluate inflammation and infection. Treatment typically starts with supportive measures like discontinuing certain medications that slow bowel function or correcting electrolyte imbalances via IV fluids. If symptoms worsen or complications begin to arise, emergency surgery may be required to remove all or part of the affected colon.
Contact Cary Gastro for Comprehensive Digestive Care
If you have inflammatory bowel disease, recurrent intestinal infections, or other digestive conditions that could potentially lead to complications, having a relationship with experienced gastroenterologists provides crucial protection. The specialists at Cary Gastro understand the importance of monitoring these conditions and recognizing early warning signs of serious complications like toxic megacolon. Our team provides comprehensive care for all digestive disorders, from routine management to emergency intervention when needed. Contact our team today to request an appointment and take a proactive approach to your digestive health.
1https://www.ncbi.nlm.nih.gov/books/NBK547679/
2https://www.hopkinsmedicine.org/health/conditions-and-diseases/toxic-megacolon