Understanding the Link Between Colorectal Cancer and Obesity
Weight loss is often on the minds of millions of Americans every day, and the motivating factor is usually related to body image and the desire to be thinner. But as the prevalence of obesity in the United States balloons past 40% of adults and adolescents, there are more fundamental factors Americans must consider. Indeed, the effects of obesity are linked to a wide variety of negative health outcomes like cardiovascular disease, hypertension, and type 2 diabetes. Another highly concerning condition that can be overlooked is colorectal cancer.
How is Obesity Defined?
Since every person’s body has a different composition, shape, and size, it can be difficult to define being overweight or obese. One tool that doctors use as a framework for defining obesity is called body mass index (BMI), a figure that is determined by a comparison of a person’s height and weight. BMI is limited in its application, however; for example, a tall man with significant muscle mass might have a higher than average BMI but not actually be obese. Nevertheless, the tool is generally a useful predictor of whether someone is underweight (BMI under 18.5), normal weight (18.5-24.9), overweight (25-29.9), or obese (30 and above).
Because of the limits inherent in BMI, there has been increased interest in another tool that can be used by doctors to help define obesity. By measuring waist circumference and waist-hip ratio, a doctor can get an even more accurate understanding of the likelihood of obesity and subsequent obesity-related conditions. This measurement is a much better indicator of fat distribution and relationship between fat mass and muscle mass.
From an overall health perspective, an important factor in defining obesity is the point at which the accumulation of adipose tissue (body fat stores) begins to have a negative impact on body systems. One of the most important examples of this is the development of insulin resistance. Insulin is an important hormone that allows cells to use glucose from dietary sources, but high-sugar and high-fat diets can reduce the effectiveness of insulin over time. Insulin resistance, then, can lead to metabolic syndrome, which is a cluster of conditions that are all related to obesity.
Obesity and Colorectal Cancer
In recent years, many large cohort studies have suggested a strong link between excess body weight and many common cancers. In fact, according to research and cancer statistics from the American Cancer Society, it is estimated that obesity is a major factor in about 7% of all cancer deaths. Yet even with all of the cancer research being done, the link with some types of cancer is not fully understood. For example, obese postmenopausal women have an increased risk of getting breast cancer compared to those who haven’t yet been through menopause.
Colorectal cancer (CRC) is another type of cancer that is strongly linked with obesity, and it is one of the most common causes of cancer death in the United States. This makes it an even greater concern as the obesity pandemic continues to grow year by year. The evidence gleaned from ongoing research shows that environmental issues like diet and activity level are key contributors to increases in colorectal cancer incidence. Research has also led to a greater understanding of how precisely obesity increases the likelihood of CRC:
- Leptin: Obesity is also known to increase both the quantity of and resistance to leptin, an adipokine hormone that regulates satiety and may spur the growth of colon cancer cells.
- Estrogen: Adipose tissue produces excess estrogen, a hormone that has been known to increase the cell growth of colorectal and many other cancers.
- Inflammation: A common concern for obese people is any number of chronic inflammatory conditions that affect different parts of the body. This kind of widespread inflammation essentially creates conditions around the body where cancer is more likely to develop.
- Insulin: As noted above, the impact of fat tissue on insulin is only now starting to be more fully understood by doctors and researchers. Fat tissue also seems to have an impact on a related hormone called insulin-like growth factor (IGF), a hormone that regulates the growth of bones and tissues.
What is Colorectal Cancer?
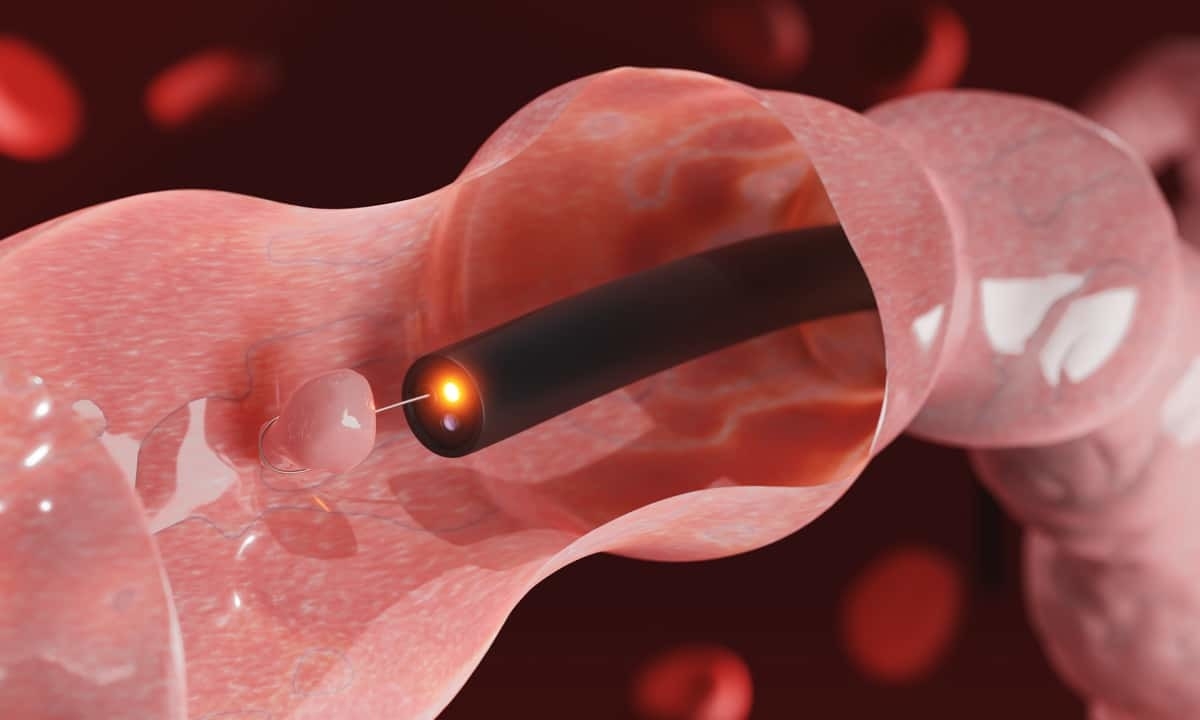
Since colon cancer and rectal cancer occur in such close proximity, and because of the similar way the two diseases progress and present, they are often referred to collectively as colorectal cancer (CRC). As with other types of cancer, CRC starts as an abnormal growth of cells; in the vast majority of cases, the abnormal growth starts as a polyp on the inner lining of the colon or rectum. Though a polyp might be benign initially, it can eventually become cancerous (a process called carcinogenesis) and is referred to as a colorectal adenoma. If left untreated, the cancerous cells can spread to other parts of the body and cause significant damage to numerous organs.
The direct cause of colorectal cancer is not fully known, but there are some risk factors that have been identified, such as smoking, heavy alcohol consumption, and a lack of physical activity. As noted above, though, obesity also significantly increases colon cancer risk; some studies have shown that obese people are 30% more likely to get colorectal cancer than those who are at a healthy weight. For reasons that aren’t currently understood, men have an even higher risk of colon cancer (up to 70%) than women.
The Effects of Weight Loss
Even though weight gain increases the relative risk of colorectal cancer, it’s not entirely borne out by research yet that weight loss necessarily decreases the risk. A meta-analysis of numerous case-control studies and observational studies, however, has suggested that avoiding weight gain in adulthood clearly reduces the chances of developing colorectal cancer or several other types of cancer. The limitations of these studies are in the fact that they aren’t often able to determine whether or not any weight loss was intentional or unintentional.
One area of research that does show a significant relationship between weight loss and reduced CRC risk is with people who have undergone bariatric surgery. Obese people who have lost weight as a result of this type of surgery have a lower risk of developing an obesity-related cancer; this seems to primarily be because of a change in certain biomarkers. Taken with other evidence currently available and what is already known about the impact of excess body fat, the clear recommendation from health care providers is that losing excess body weight can only be beneficial.
The key to cancer prevention is making modifications to lifestyle factors that are in your control and can have an impact on your risk profile. This is especially true for anyone who has a family history of colorectal cancer; though research is still ongoing about the genetic implications, there does seem to be a greater risk if a family member has cancer. Making modifications to your diet and increasing your physical activity level are two ways anyone can start, but depending on your BMI and waist circumference, there may be other medical and surgical options for losing weight.
Contact Cary Gastro
At Cary Gastro, our dedicated doctors and staff are passionate about providing excellent digestive healthcare. Colorectal cancer is on the rise in the U.S. and obesity is clearly driving some of this growth. One of the best tools to stay ahead of a potential development is cancer screening via a colonoscopy. If you would like more information about colorectal cancer or getting screened, please contact us to request an appointment.