What to Know About Esophageal Achalasia
All day, every day, the various muscles in our body contract and relax based on our conscious decisions or regular autonomic functions. Sometimes, though, certain muscles have trouble relaxing after contraction; this abnormal function can cause a number of symptoms and additional health problems. One somewhat rare example of this is the condition known as achalasia. While achalasia can potentially occur with smooth muscle anywhere in the body, the most common location is in the esophagus, the hollow tube that connects the mouth to the stomach.
Achalasia and the Esophagus
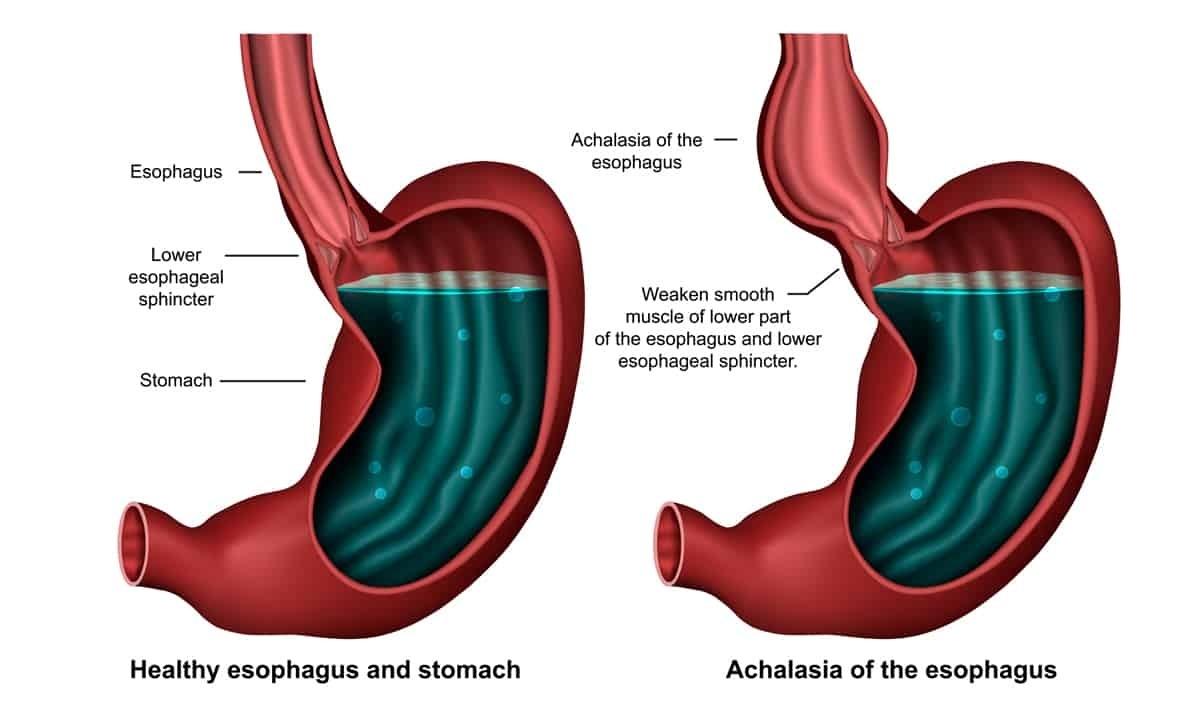
During the normal course of the digestion process, chewed up food is swallowed and enters the esophagus. Smooth muscle surrounding the esophagus helps push the food mass down through a process called peristalsis. At the bottom end of the esophagus, the lower esophageal sphincter (LES) separates the lower esophagus from the stomach. When food reaches this point, the LES relaxes so the food can move into the stomach; the LES then contracts in order to prevent food and stomach acid from backing up into the esophagus.
In patients with esophageal achalasia, however, the lower esophageal sphincter is unable to relax. This prevents recently swallowed food from actually making it into the stomach. In addition to LES malfunction, the muscle surrounding the rest of the esophagus has reduced or impaired function, including peristalsis. Achalasia is a relatively rare condition that affects about 1 in 100,000 each year. Anyone can develop achalasia, though it is most common in men and women ages 25 to 60.
Causes of Achalasia
Unfortunately, not much is known about the underlying reason for why the esophageal muscles begin to malfunction. Given that the lower esophageal sphincter is regulated by neurotransmitters from the enteric nervous system, one possible explanation is that achalasia is an autoimmune response. In this theory, a virus or other pathogen infects the lining of the esophagus; the immune system detects this pathogen and inadvertently attacks nerve cells in the muscle layers of the esophagus. This then leads to excessive contractions and an inability to subsequently relax.
More research is needed to truly understand this condition, however. While achalasia may be an autoimmune condition, it may not occur because of infection. There is some evidence that the condition is genetic and therefore passed on from a family member. Although not a candidate for an underlying cause, there is a rare tropical parasitic illness called Chagas disease that is spread by insects in Central and South America. The presence of the parasite in the body triggers an autoimmune response that can lead to the development of achalasia.
Symptoms of Achalasia
The main symptoms of achalasia are due to the direct physical impact of lower esophageal sphincter not relaxing. When this happens, solids and liquid cannot enter the stomach to continue to progress through the gastrointestinal tract; food backs up in the esophagus and often causes regurgitation. If left untreated, the symptoms worsen over time and serious complications may follow. Below are some common symptoms of achalasia:
- Dysphagia: one of the most common symptoms, dysphagia means difficulty swallowing, usually due to a narrowing of the esophagus
- Regurgitation: food backed up in the esophagus by a malfunctioning LES can pushed up into the back of the throat
- Chest pain: also known as cardiospasm, the chest pain experienced with achalasia can be mistaken for a heart attack and may also be felt in the back, neck, or arms
- Unintentional or unexplained weight loss
- Coughing
- Dry eyes or mouth
- Pain or discomfort after eating
In many cases, the symptoms of esophageal achalasia can essentially mimic the symptoms of acid reflux (heartburn) and its chronic counterpart, gastroesophageal reflux disease (GERD). Both GERD and achalasia are influenced by the malfunction of the lower esophageal sphincter, but in GERD the LES has trouble closing while in achalasia the LES has trouble opening. In each case, though, the disruption to the digestive process yields some similar results. There is also evidence that people may be more susceptible to achalasia after having GERD.
Complications of Achalasia
If left untreated, one of the more extreme complications or side effects of achalasia is the phenomenon known as megaesophagus. When the LES stays closed for too long, backed up food stretches the esophagus to the extreme. Most people are unaware of the blocked passage and will continue to eat and drink while the esophagus continues to swell. The resulting nausea eventually leads to an uncontrollable urge to vomit. In some situations, the regurgitated food can become drawn into the trachea; the bits of partially decayed food can then cause a lung infection or pneumonia.
One of the other complications of achalasia that can be a major concern is also related to the condition being left untreated. In cases where the lower esophageal sphincter is tightly closed, literally no food or water can be broken down by the stomach or absorbed by the intestines. Without medical intervention, the condition can progress from rapid weight loss to starvation and death fairly quickly. Moreover, severe or repeated instances of achalasia can also increase your risk of developing esophageal cancer.
Diagnosis of Achalasia
Because achalasia has similar symptoms as GERD and some other gastrointestinal conditions, diagnosis sometimes requires multiple steps. One of the most common tests used to diagnose achalasia is an X-ray with a barium swallow. The patient is given a barium solution (usually in liquid form) to ingest; barium is used as a contrast medium so that abnormalities in the gastrointestinal tract can be more easily observed during an X-ray.
Another very common test is upper endoscopy. In this test, the doctor feeds the long, flexible endoscope down the esophagus to look for problems in the esophagus. The mounted camera allows direct visual examination, and small tools allow the doctor to collect a sample for biopsy or even remove lesions. If visual tests are still inconclusive, esophageal manometry is another option. Through a carefully placed catheter, this test measures the motor function and timing of the lower esophageal sphincter. This test can help a doctor determine whether or not the LES is properly relaxing in response to swallowing.
Treatment of Achalasia
There is unfortunately no known cure for achalasia, but there are a variety of treatment options for easing or managing the symptoms. In some cases, treatment can also improve the relaxing function of the LES and prevent additional complications. Below are some of the standard options available to doctors:
- Pneumatic dilation: during this outpatient endoscopic procedure, a special balloon is placed in the esophagus and inflated; also known as balloon dilation, the procedure stretches out the esophagus and eases symptoms like dysphagia
- Botulinum: a botulinum toxin injection can be used to essentially paralyze the muscles of the LES and improve its ability to relax and open
- Surgery: the primary surgical option to treat achalasia is a laparoscopic Heller myotomy and it involves making incisions to the outer layer of muscles in the LES that keep it closed; this procedure is often paired with a partial fundoplication in order to promote efficient function and reduce the likelihood of developing GERD
- POEM: peroral endoscopic myotomy (POEM) is an alternative surgery that is performed entirely with an endoscope; though the end result is similar, the use of an endoscope makes it a safer procedure with a quicker recovery time
- Medication: either calcium channel blocker or long-acting nitrates may be prescribed if some other interventions are not successful
When to Contact a Gastroenterologist
As noted, the symptoms of achalasia can sometimes be mistaken for GERD or another gastrointestinal condition. If you’ve experienced difficulty swallowing, food regurgitation, or any of the symptoms listed above and they’ve been getting worse, it may be time to see a gastroenterologist. At Cary Gastro, our dedicated staff is passionate about providing excellent digestive healthcare so you can have maximum quality of life. Please contact us today for more information or to request an appointment.