What You Need to Know About Pancreatic Cancer
According to the American Cancer Society, the U.S. will see nearly two million new cancer cases and over 600,000 cancer deaths by the end of this year. The good news is that the overall incidence of cancer has been going down in the last few years, but unfortunately there are some types of cancer that have been trending the opposite way. One prominent example of this is pancreatic cancer; even though it only accounts for 3% of all cancer cases, pancreatic cancer accounts for 7% of all cancer deaths.
What Does the Pancreas Do?
The pancreas is a small, elongated organ found in the abdominal cavity just behind the stomach. One notable feature of the pancreas is that it can be considered as part of the digestive system and as part of the endocrine system. As far as what purpose it serves, it can best be thought of in two categories: endocrine and exocrine:
Endocrine Function: The term endocrine refers to substances being produced and secreted directly into the bloodstream. The pancreas does this through a cluster of cells called the islets of Langerhans; messenger hormones released here are important in digestion and more specifically in the regulation of blood sugar:
- Insulin: Produced by beta cells in the pancreas, insulin is one of the most important hormones in the process of metabolizing glucose and keeping blood sugar from being too high. When glucose is present in the digestive system, insulin secreted by the pancreas is triggered in order to enable cells to use the glucose for energy needs.
- Glucagon: Another significant part of the pancreas’ endocrine function is in the production of glucagon, a peptide hormone that is crucial in preventing blood sugar levels from getting too low. Glucagon is produced by alpha cells in the pancreas, and its secretion tells the liver to release stored glucose into the bloodstream.
- Additional hormones: The pancreas also produces small amounts of amylin and gastrin, two hormones that regulate the gastric acid production, stomach emptying, and appetite control.
Exocrine Function: The term exocrine, by contrast, refers to substances that are secreted and released by a duct. In the case of the pancreas, enzymes are produced and travel to the digestive tract via pancreatic ducts. These enzymes are part of the digestive juices that break down food so that the nutrients can be absorbed by the small intestine:
- Lipase: Along with bile produced in the liver, the enzyme lipase breaks down fat molecules into usable form. It is important, for example, in the digestion of fat-soluble nutrients like vitamin A and vitamin K.
- Protease: Protease is a similarly valuable enzyme that is involved in the breaking down of proteins into essential amino acids. It also helps protect the body from pathogens by boosting immune function.
- Amylase: Amylase is also crucial for digestion because it is an enzyme that breaks down carbohydrates so that they can meet the body’s energy needs.
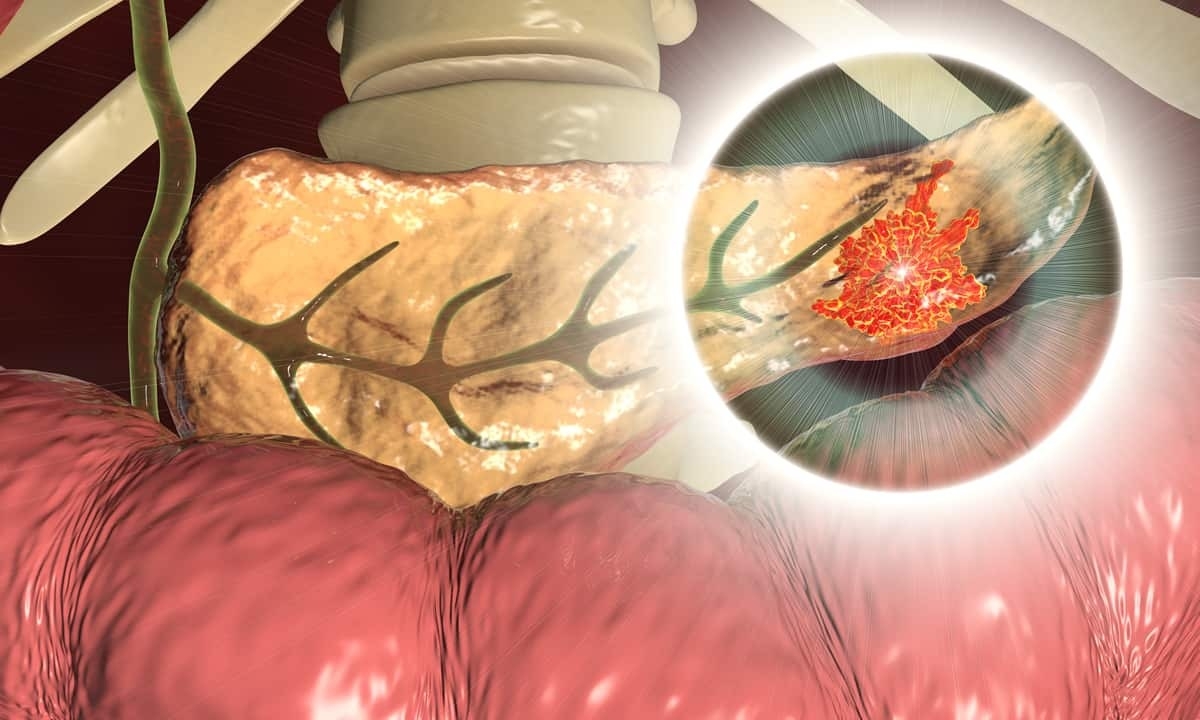
What Is Pancreatic Cancer?
Pancreatic cancer is so named because it begins in the pancreas, but it is the same as all cancers in that it starts with the abnormal growth of cells that leads to mutations. Any of the cells in the pancreas can potentially lead to overgrowth and cancer, but pancreatic tumors are more likely to form in the cells related to exocrine function rather than those related to endocrine function. Below are some of the most common types of pancreatic cancer:
- Pancreatic adenocarcinoma: The vast majority (over 90%) of all cases of pancreatic cancer are known as ductal adenocarcinoma. This type develops in the lining of the various ducts that are spread out within the pancreas.
- Acinar cell carcinoma: Though rarer (about 5% of cases), acinar cell carcinoma is the second most common type of pancreatic cancer. Acinar cell carcinoma is also an exocrine cancer, and it develops in the cell clusters that are responsible for producing pancreatic enzymes.
- Squamous cell carcinoma: Squamous cell carcinomas and adenosquamous carcinomas are also a fairly rare (around 1-2% of cases) type that develops in squamous cells that aren’t normally found in the pancreas. These tend to be much more aggressive and have a poorer prognosis.
- Neuroendocrine tumors: Whereas most types of pancreatic cancer come from exocrine cells, pancreatic neuroendocrine tumors come from endocrine cells in the islets of Langerhans; this is why they are also sometimes referred to as islet cell tumors. This type represents less than 5% of cases of pancreatic cancer.
- Colloid carcinoma: A colloid carcinoma comes from benign cysts that contain mucin, a gelatinous substance that makes the cancer less likely to spread; it is therefore also easier to treat.
- Ampullary cancer: Ampullary cancer and periampullary cancer develop in or near the ampulla of Vater, an important junction where the pancreatic duct and common bile duct unite and connect and interact with the duodenum. While they don’t arise in the pancreas specifically, they are related and are typically treated in the same way.
Symptoms of Pancreatic Cancer
Like most other types of cancer, the early stages of pancreatic cancer don’t usually present with any notable symptoms. In fact, by the time cancer symptoms do become apparent, the cancer cells have likely spread to areas outside the pancreas. However, one of the earliest symptoms is jaundice, a yellowing of the skin and eyes that is caused by a blockage in the common bile duct. If left undiagnosed and untreated, symptoms can also eventually include abdominal pain, unexplained weight loss, nausea, vomiting, and a lack of appetite.
Risk Factors for Pancreatic Cancer
Doctors don’t really know what causes the abnormal growths that can lead to pancreatic cancer, but a number of risk factors have been identified. It is much more likely to develop, for example, as people get older; in fact, almost all pancreatic cancer patients are over the age of 45. It is also more likely to develop in men than women. While some of these factors are inherent and can’t be changed, there are also some that are related to lifestyle:
- Smoking: People who smoke are nearly twice as likely to get pancreatic cancer as those who don’t smoke, but this risk drops dramatically as soon as a person stops smoking.
- Obesity: People with a body mass index (BMI) of 30 or higher are about 20% more likely to develop pancreatic cancer.
- Diabetes: While the connection is not fully understood, research shows that people with type 2 diabetes are at a higher risk of pancreatic cancer. Moreover, type 2 diabetes also often associated with being obese or overweight.
- Pancreatitis: Pancreatitis refers to an inflammation of the pancreas that can occur for a variety of reasons. Chronic pancreatitis can then lead to scarring and fibrosis that is thought to be a pathway to malignancy.
Pancreatic Cancer Treatment Options
Before a course of treatment is determined, a doctor of oncology must make a pancreatic cancer diagnosis. Because it is difficult to detect this type of cancer early on, the doctor may look to imaging tests like an endoscopic ultrasound or cholangiopancreatography, a type of MRI that looks specifically at pancreatic and biliary ducts. In some cases an endoscope may be used to biopsy a tissue sample to test for cancer. There are also some markers for tumors that can be detected through a blood test.
Once cancer has been diagnosed, the treatment will depend on the specific type of pancreatic cancer and the extent to which it has spread. If it is still early on, it may be possible to eliminate the cancerous cells. If the cancer is at a more advanced stage, though, the options may be limited to preventing the further spread or improving quality of life. Below are some common treatment options:
- Surgery: Surgery is the main option when the tumor is resectable, which means that it has stayed in the pancreas in a defined area and can be fully removed. Depending on where the cancerous cells are located, the surgeon can either use a distal pancreatectomy or a Whipple procedure to remove any tumors.
- Chemotherapy: If surgery either isn’t an option or didn’t work, chemotherapy drugs are typically the next step. These drugs are delivered intravenously and are designed to kill cancer cells, but they can also have challenging side effects like hair loss, fatigue, and a compromised immune system.
- Radiation therapy: Radiation therapy is often used in conjunction with chemotherapy in cases where surgery isn’t an option or wasn’t able to remove all the cancerous cells. Radiation therapy is also used in clinical trials with other types of therapy like immunotherapy or vaccines.
Request an Appointment With a Gastroenterologist
As alluded to above, it’s very possible to have pancreatic cancer without knowing about it because of a lack of symptoms. If you think you might have pancreatic cancer, or if you have other symptoms related to the digestive system, contact Cary Gastro to request an appointment. We are passionate about providing excellent digestive health care so that you can have peace of mind and a maximum quality of life.