Can Hemorrhoids Lead to Colorectal Cancer?
Men and women of all ages can get hemorrhoids, but the likelihood goes up substantially after age 50. This decidedly unpleasant condition is commonly associated with symptoms like swelling, pain, and irritation, yet it usually can be managed through a number of effective remedies. In more advanced cases, however, the symptoms may be persistent or more severe. Some of these symptoms, like rectal bleeding, can even mimic the symptoms of much more serious conditions. One example of such a condition is colorectal cancer, but can hemorrhoids actually lead to cancer?
What Are Hemorrhoids?
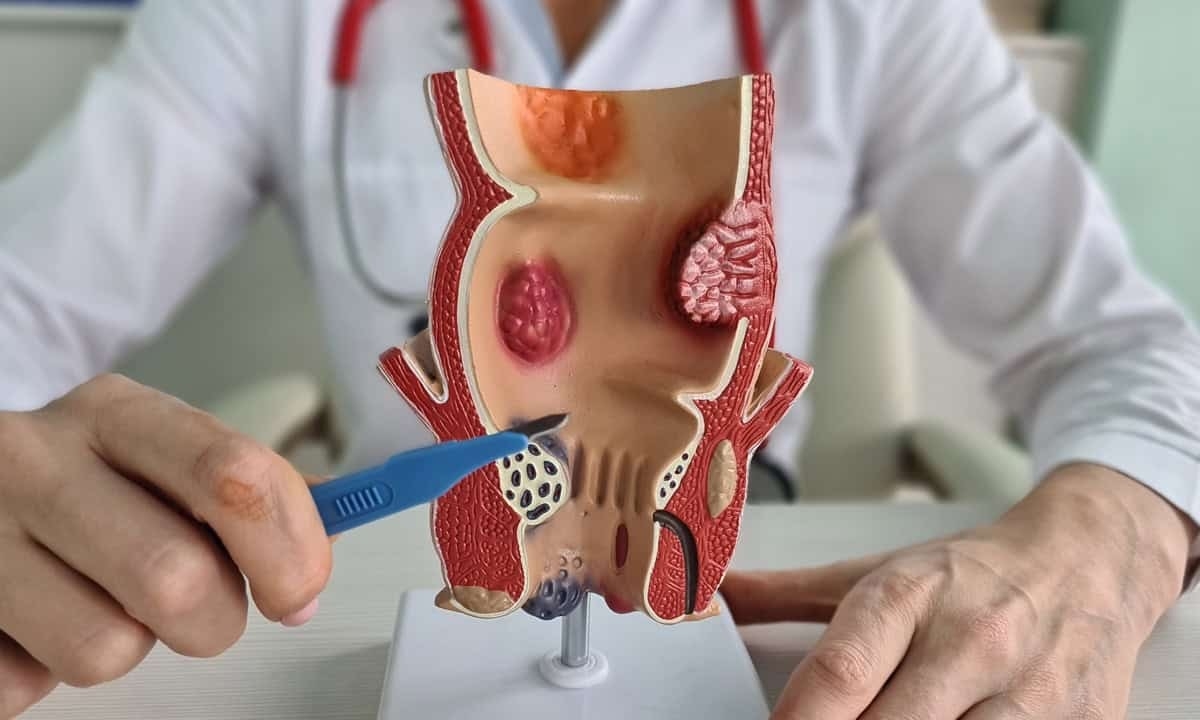
Hemorrhoids develop when blood vessels in the anal area and lower rectum become swollen and enlarged beyond their normal size. While everyone has these blood vessels as part of normal anatomy, they become problematic when increased pressure causes them to expand and create uncomfortable symptoms. The location determines the type: internal hemorrhoids develop inside the rectum where they often cause painless bleeding during bowel movements, while external hemorrhoids form under the skin around the anal opening and tend to be more painful, especially when blood clots develop within them.
The underlying causes of hemorrhoids typically involve sustained pressure on the blood vessels in the pelvic area. Chronic constipation creates a cycle where people strain during bowel movements, which increases pressure on these already vulnerable blood vessels. A diet low in fiber contributes to this problem by producing harder stools that require more effort to pass, while obesity adds extra weight that affects blood circulation throughout the pelvic region. Pregnancy is a particularly common trigger, as the growing baby creates physical pressure while hormonal changes simultaneously weaken blood vessel walls. Even habits like prolonged sitting, particularly on the toilet while reading or using a phone, can impede normal blood flow and contribute to hemorrhoid development over time.
When hemorrhoids become symptomatic, they typically produce rectal bleeding that appears bright red and occurs during or shortly after bowel movements. Pain levels vary considerably depending on location and severity, with external hemorrhoids generally causing more discomfort than their internal counterparts. Many people also experience itching around the anal area or a persistent feeling that bowel movements are incomplete. These symptoms result from the mechanical effects of enlarged blood vessels rather than from cellular changes that characterize cancer development.1
The Connection Between Hemorrhoids and Cancer
The concern about a potential link between hemorrhoids and cancer often stems from the overlap in symptoms that these conditions can produce. This symptom overlap becomes particularly concerning when people experience rectal bleeding for the first time or notice changes in bowel movements. Colorectal cancer, anal cancer, and rectal cancer can all present with bleeding and discomfort that might initially seem consistent with hemorrhoid symptoms. The similarity in presentation means that distinguishing between these conditions often requires professional medical evaluation rather than self-diagnosis.
Despite these shared symptoms, hemorrhoids themselves do not cause cancer or transform into cancerous tissue. Hemorrhoids develop when blood vessels become enlarged due to mechanical pressure, similar to how varicose veins form in the legs. The tissue remains normal vascular tissue that has become swollen and inflamed. Cancer involves an entirely different process where genetic mutations cause cells to grow uncontrollably, representing a fundamental cellular change rather than simple swelling of existing structures.
Managing Hemorrhoid Symptoms
While hemorrhoids can be uncomfortable and concerning, most patients respond well to conservative treatment approaches that address both symptoms and underlying causes. The goal of treatment focuses on reducing pressure on the affected blood vessels while providing relief from pain, swelling, and irritation. Many people find significant improvement through lifestyle modifications combined with over-the-counter remedies, though persistent or severe symptoms may require medical intervention. Effective hemorrhoid management typically involves several complementary approaches:
- Dietary modifications: Increasing fiber intake through fruits, vegetables, and whole grains helps soften stools and reduce straining during bowel movements. Adequate hydration supports healthy bowel function and prevents constipation that can worsen hemorrhoid symptoms.
- Bathroom habits: Avoiding prolonged sitting on the toilet and responding promptly to the urge for bowel movements can reduce pressure on anal blood vessels. Using a footstool to elevate the knees during bowel movements may also help reduce straining.
- Topical treatments: Over-the-counter creams, ointments, and suppositories containing ingredients like hydrocortisone or witch hazel can provide temporary relief from pain and itching. These treatments address symptoms but don’t cure the underlying condition.
- Sitz baths: Soaking the anal area in warm water for 10-15 minutes several times daily can reduce inflammation and provide comfort. This simple treatment improves blood flow and can accelerate healing of irritated tissue.
- Physical activity: Regular exercise promotes healthy bowel function and circulation while helping maintain a healthy weight that reduces pressure on pelvic blood vessels.
Complications and When to See a Doctor
In most cases, the standard treatments are effective at controlling hemorrhoids and easing the symptoms. There are, however, some complications and warning signs that indicate the need for professional medical evaluation. One of the most painful complications is thrombosed hemorrhoids; this is when blood clots form within external hemorrhoids and create severe pain that typically doesn’t respond to over-the-counter treatments or sitz baths. The clots can cause significant swelling and may require medical procedures to provide relief. Another example is prolapsed hemorrhoids that require medical treatment to resolve.
Beyond specific complications, it is also a concern if the symptoms persist or worsen even after several weeks of traditional treatments. This includes bleeding that continues or increases, pain that interferes with daily activities, or new symptoms that develop during treatment. Additionally, certain warning signs suggest the possibility of conditions more serious than hemorrhoids. Unexplained weight loss accompanying rectal bleeding should prompt immediate medical consultation, as should persistent changes in bowel habits that don't improve with dietary modifications. Dark or black stools, severe abdominal pain, or bleeding between bowel movements rather than only during them may indicate problems beyond simple hemorrhoids.
Contact Cary Gastro for Hemorrhoid Relief
While hemorrhoids are common and generally not serious, persistent symptoms may call for professional evaluation to rule out more concerning conditions. The experienced gastroenterologists at Cary Gastro provide comprehensive assessment of rectal bleeding and other gastrointestinal symptoms, using advanced diagnostic techniques to distinguish between hemorrhoids and other conditions. Our team understands the anxiety that accompanies these symptoms and provides thorough, compassionate care to ensure accurate diagnosis and appropriate treatment. Contact us today to request an appointment and get the expert evaluation you need.
1https://www.niddk.nih.gov/health-information/digestive-diseases/hemorrhoids/definition-facts