What to Know About Familial Adenomatous Polyposis
According to the American Cancer Society, the lifetime risk of colorectal cancer is about 4% and 3% for men and women, respectively. As with most other types of cancer, the precise mechanisms that cause the disease are still unclear. What is clear about cancer in general, however, is that genes seem to play a significant role in who gets it. One example of a genetic condition that is known to lead to either colon cancer or rectal cancer is called familial adenomatous polyposis.
What Is Familial Adenomatous Polyposis?
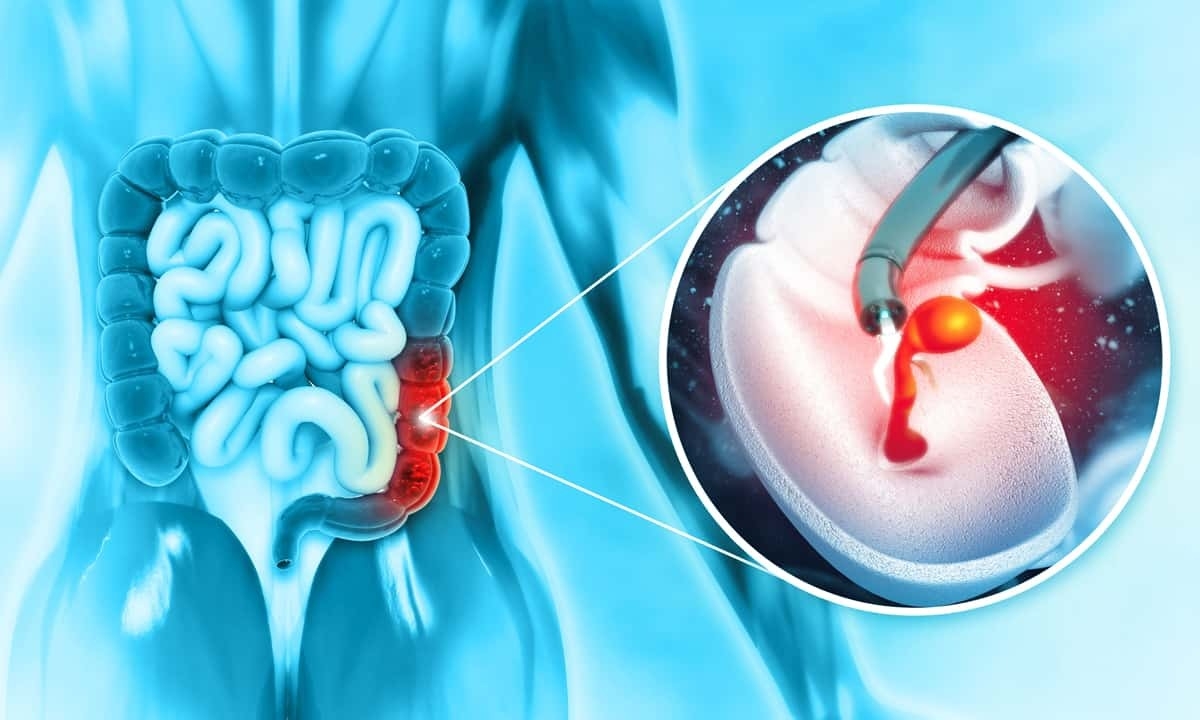
Familial adenomatous polyposis (FAP) is a rare genetic disorder characterized by the development of numerous adenomatous polyps in the colon and rectum. FAP is considered an autosomal dominant condition because an individual only needs one copy of the mutated gene from either parent to develop the disorder. As noted above, familial adenomatous polyposis is also strongly linked with colorectal cancer; in fact, even though only about 1% of colorectal cancer cases are due to FAP, nearly 100% of cases of FAP will lead to colorectal cancer.
Familial adenomatous polyposis is primarily caused by mutations in a particular gene known as adenomatous polyposis coli (APC). As a tumor suppressor gene, APC is responsible for controlling cell growth in the lining of the colon. This is one of the body’s main ways of preventing growths and other abnormalities from forming in the body. As a result of APC gene mutation, though, there is a greatly increased risk of colon polyps forming in the large intestine. If left untreated, there is a similarly high risk of colorectal cancer developing.
As an inherited genetic condition, FAP is present from birth, but it doesn’t typically become apparent until later childhood or adolescence. Usually by the teenage years, benign growths may start to form in the colon, and then the average age when colon cancer can begin to develop is around 39-40 years of age. How it develops and the symptoms that present are then somewhat dependent on the variant of FAP and the number of polyps involved:
- Classic FAP: “Classic” FAP is the most common and well-known form of this cancer syndrome, and it involves the formation of hundreds of adenomatous polyps in the colon and rectum. While initially benign, these colorectal polyps can and usually do become malignant.
- Attenuated FAP: Attenuated familial adenomatous polyposis (AFAP) is considered a milder form of the condition mainly because the number of polyps found in the colon is fewer than in classic FAP; it typically ranges from 10-100 polyps. Even though this type tends to occur later in life and involves fewer polyps, it still has only a slightly reduced risk of colorectal cancer.
- MUTYH-associated polyposis: Also known as MYH-associated polyposis syndrome, this subtype is similar to FAP; but unlike FAP, which is related to APC gene mutation, this condition is caused by a mutation of MUTYH, a gene associated with repairing oxidative damage in DNA. As with other types, the condition generally leads to the development of adenomas in the gastrointestinal tract; in this case, though, various growths can occur inside the colon as well as in the duodenum and other parts of the small intestine.
- Gardner syndrome: Gardner syndrome is another subtype of FAP with the same kind of development of adenomatous polyps in the colon and rectum. The main differentiating factor is that the person develops related extracolonic manifestations elsewhere in the body; examples of these manifestations are osteomas, desmoid tumors (a type of soft tissue tumor), epidermoid cysts, or a rare eye condition called congenital hypertrophy of the retinal pigment epithelium (CHRPE).
- Turcot syndrome: Turcot syndrome is a rare cancer syndrome that involves the formation of polyps in both the gastrointestinal tract and structures of the central nervous system. People with Turcot thus have a predisposition to both colorectal cancer and brain tumors from a young age.
- Lynch syndrome: Lynch syndrome is technically known as hereditary nonpolyposis colorectal cancer (HNPCC), and it is a hereditary genetic condition that increases the risk factors of colorectal cancer and several other types of cancer. Lynch syndrome is similar to Turcot in that it is caused by mutations in genes that are involved in DNA mismatch repair.
How Is Familial Adenomatous Polyposis Diagnosed?
Given that familial adenomatous polyposis is a genetic condition, any diagnosis of FAP will necessarily stem from an evaluation of a patient’s family history. Because of this, genetic testing is a key component of the diagnostic process, and the goal is to identify potential mutations of the APC gene. Such tests are usually followed by genetic counseling in order to discuss the implications of the results and the likelihood of developing cancer. There may also be an evaluation of any symptoms already present.
One of the most important steps for verifying the condition is to use one or more endoscopic imaging studies. A colonoscopy or sigmoidoscopy are key diagnostic tools because they allow a doctor to directly visualize the inner lining of the colon to look for polyps. In some cases, an upper endoscopy may also be used to assess the presence of polyps in the upper gastrointestinal tract. If polyps are discovered during these procedures, tools on the end of the scope can take tissue samples for a biopsy.
Treatment Options
The treatment of familial adenomatous polyposis is primarily aimed at managing the symptoms, preventing the progression of polyps to colorectal cancer, and addressing any associated complications. The treatment approach for FAP often involves a combination of surveillance, medications, and, in some cases, surgical interventions:
- Surveillance: Especially when any family members have previously been diagnosed, it is important to begin regular colonoscopies as early as adolescence. How often a colonoscopy is recommended will depend in part on the number and size of polyps found in the gastrointestinal tract.
- Medication: Research into effective medications is ongoing, but there is some evidence that non-steroidal anti-inflammatory drugs (NSAIDs) may decrease the overall number of polyps; however, so far this effect may be limited since it doesn’t seem to decrease the number enough to treat endoscopically. Other drugs, such as celecoxib and sulindac, may be able to be used in combination with NSAIDs for a better outcome.
- Surgery: Unfortunately, the fact that FAP has such a strong link to colorectal cancer means that some patients will require surgery to either excise cancer cells or to preemptively prevent cancer from growing. The most common type of surgery performed in these cases is a partial or total removal of the colon (colectomy). Removal of the colon typically also means the creation of an ileal pouch or stoma in cases where bowel function is impaired by the surgery.
Get Screened at Cary Gastroenterology
Familial adenomatous polyposis is a rare condition that only affects a segment of the population that has a genetic predisposition. But even if you don’t have FAP, the fact is that colorectal cancer is still one of the most common and deadly forms of cancer. Guidelines from the American College of Gastroenterology and other groups now recommend regular cancer screenings for adults 45 and older, or younger if you also are at a higher risk for any reason. At Cary Gastro, we are passionate about long-term digestive health. If you haven’t been screened for colon cancer yet, or if you want to talk with a gastroenterologist about any symptoms, please contact us today to request an appointment.